Integrated Dual Diagnosis Treatment in Massachusetts Designed for Lasting Recovery
When Mental Health and Addiction Collide, You Deserve Care That Treats Both

Why Dual Diagnosis Treatment Centers in Massachusetts Are Needed
For Massachusetts residents working towards full recovery from both substance use and mental health disorders, the intersection of these two areas creates complex challenges.
Addiction-related research suggests that more than half of people who have a substance use disorder also experience one or more other mental health diagnoses, such as Major Depressive Disorder (MDD), Anxiety Disorders, Post Traumatic Stress Disorder (PTSD), and Bipolar Disorder.[1] Integrated treatment options for dual diagnosis remain underutilized in Massachusetts despite studies showing significantly better outcomes for patients who receive integrated care for both a substance use disorder and related mental health disorder as opposed to treating each disorder alone.[2]
The existence of this treatment gap can be attributed, in part, to facilities treating these disorders separately and making people turn to two different providers to treat substance use disorders and mental health disorders. Standard treatment models for substance use view the psychiatric symptoms associated with substance use as “secondary issues” that must be dealt with after the person is sober, while standard treatment models for mental health often refuse to engage patients in care until they are sober. This dichotomy in care creates a system that “bounces” patients between tiers without providing comprehensive care to meet the individual needs of the patient for long-term recovery and rehabilitation.
Dual Diagnosis Treatment Centers exist to bridge this gap by offering integrated care and coordinating treatment for individuals who are experiencing a dual diagnosis.
What Is Dual Diagnosis Treatment?
Dual Diagnosis is the provision of simultaneous substance use treatment and psychiatric treatment combined within a unified framework. Rather than attempting to treat two disorders (i.e., substance abuse and mental health) as distinct from one another, Dual Diagnosis programs recognize that both conditions often influence and exacerbate each other in a manner that will require simultaneous intervention.
The link between mental health and substance use can be attributable to a variety of interrelationships. Some individuals may become addicted to a substance to self-medicate an underlying or untreated mental health condition, e.g., using alcohol to relieve anxiety; using opiates to numb their emotional pain; or using a combination of stimulants to alleviate their depression-induced lethargy.[3] Alternatively, some individuals may experience mental health problems as a result of chronic addiction—depression by virtue of alcohol as a depressant or anxiety as a result of using stimulants. Many individuals will present with a combination of both paths, where each problem is exacerbated by the other, creating self-perpetuating cycles.
Therapeutic approaches utilized during treatment for addiction may not be appropriate or safe when treating patients with severe depression or a psychotic disorder, and certain psychiatric medications also warrant a higher level of precaution than would otherwise be given for a person with an active addiction. Dual Diagnosis Programs utilize their combined knowledge in both treatment areas to safely and effectively navigate the complexities involved in treating both substance use and related mental health disorders.
Who Is a Candidate for Dual Diagnosis Treatment Programs?
For patients with both mental health and alcohol/substance use disorders, the identification of the need for an integrated dual diagnosis treatment plan or treatment process, rather than a standard addiction treatment process or standard mental health treatment process, may afford individuals the ability to achieve their highest potential in recovery.
The Existence of Severe Mental Health Symptoms During Sobriety
Studies indicate that if a person is experiencing significant mental health symptoms and does not receive proper care for those symptoms, their risk for relapse is increased exponentially because, in an attempt to “medicate” themselves, they often will return to the use of substances.[4]
Using Substances as Self-Medication
Individuals may recognize that they use substances specifically to help keep their mental health symptoms under control (e.g., drinking alcohol to sleep or reduce anxiety; using stimulants to counteract depression; using opiates to numb their emotional pain). These individuals are in a position to benefit from a dual diagnosis treatment approach that addresses both their substance use disorder and any underlying mental health diagnosis. It may be extremely difficult to stay clean and sober when an individual has not adequately treated the root cause(s) of their substance use.
Previous Treatment Failures
People who have gone through an addiction recovery program and/or received treatment for mental health issues but have not improved following treatment will also benefit from receiving an integrated approach to their recovery. For instance, if a person was able to attain sobriety while receiving Residential Treatment, but relapsed within a matter of weeks after returning home, they may have a mood disorder (i.e., MDD or anxiety) that had not been treated appropriately and would have negatively impacted their ability to sustain sobriety from alcohol.
Similarly, if an individual were to receive treatment for a psychiatric condition such as Major Depressive Disorder (MDD) without addressing their ongoing substance use, that individual will often fail to make significant improvements in their treatment for MDD. This is due to the fact that while an individual is actively using substances, they often do not receive the full benefit of their medications, and their therapeutic progress is hindered due to the interference of their substance use.
Trauma History
The relationship between trauma and mental health as well as substance abuse is a well-established correlation. Therefore, those individuals who have significant trauma histories (e.g., childhood physical/sexual abuse, combat veterans, rape survivors, etc.) will benefit from a dual diagnosis treatment approach that includes trauma-informed care as well as addressing substance use.
Elements of Dual Diagnosis Treatment
In order for a treatment program for co-occurring disorders to be effective, it must utilize multiple therapeutic modalities/approaches that work in harmony to address both disorders.
Integrated Assessment and Treatment Planning
The initiation of dual diagnosis treatment begins with a thorough assessment conducted by professionals who are trained to provide treatment for both substance use disorders and co-occurring mental health disorders. The assessment will look at the individual’s history and patterns of substance use as well as their psychiatric symptoms and diagnosis, their trauma history, their mental health history, their past experiences with treatment, their current medications, and how, if at all, the co-occurring conditions impact each other and/or the person’s addiction. The comprehensive nature of this assessment will allow for clinicians to prepare an integrated treatment plan that prioritizes the most appropriate interventions and provides the sequencing of those interventions so as to maximize their effectiveness.
Robust Psychiatric Services and Medication Management
Dual diagnosis treatment centers typically provide a full range of psychiatric care, including the evaluation of individuals by Medical Doctors and/or Psychiatric Nurse Practitioners, to determine the best course of treatment depending upon the individual’s current mental health status. The psychiatric staff will evaluate the efficacy and side effects of medications prescribed for depression, anxiety, bipolar disorder, psychosis and/or other co-occurring disorders. They will also provide medication-assisted treatment for individuals who meet specific criteria and provide the prescribing psychiatrist and therapist with the necessary clinical information regarding the interactions among medications used to treat co-occurring conditions.
Evidence-Based Therapy
There are many therapeutic modalities available that treat dual diagnosis. Cognitive behavioral therapy focuses on a person’s distorted cognitive patterns that affect both substance abuse and psychiatric disorders, and teaches people coping skills that can be used for both substance abuse and psychiatric challenges. Additionally, cognitive behavioral therapy helps a person identify their triggers and develop alternative responses to those triggers. Dialectical Behavioral Therapy (DBT) was developed primarily for people suffering from Borderline Personality Disorder (BPD) and provides an individual with skills to manage their behaviors and emotions in order to develop mindfulness and to learn how to communicate effectively. In addition to BPD, DBT has been identified as providing significant benefits to persons dealing with other co-occurring disorders as well.
Trauma-focused therapies (such as Eye Movement Desensitization and Reprocessing Therapy and Trauma-Based Cognitive Behavior Therapies) are beneficial in helping people process experiences of trauma that often contribute to mental health and addiction disorders. These types of therapies provide a safe and supportive environment to address trauma experiences that traditional addiction counseling lacks.
Motivational Interviewing provides a means for people with co-occurring disorders to identify and work through their feelings of ambivalence towards creating positive change in both areas, and ultimately strengthens the individual’s commitment to both recovery from substance use and management of the psychiatric disorder.
Individualized Treatment
Persons with co-occurring disorders generally require an increased intensity or length of treatment than persons whose only disorder is an addiction. Dual diagnosis programs typically offer an extended residential treatment program, extended time periods to participate in partial hospitalization and intensive outpatient programs, increased frequency of individual therapy sessions, as well as continued psychiatric monitoring and a gradual step-down from one level of care to another. The extra time spent in dual diagnosis programming allows both conditions to stabilize prior to discharge from intensive care settings and transition to less intensive support.
Prevention Plans for Dual Diagnosis Recovery
Relapse prevention in dual diagnosis treatment must address both conditions. A plan will identify the triggers for both the substance abuse and worsening of psychiatric symptoms, develop coping strategies to manage cravings and mental health symptoms, recognize the early warning signs that a relapse may occur in either area and create an action plan to follow when either of these two areas become problematic, build support systems for both areas of concern, and maintain consistent medication adherence for both areas.
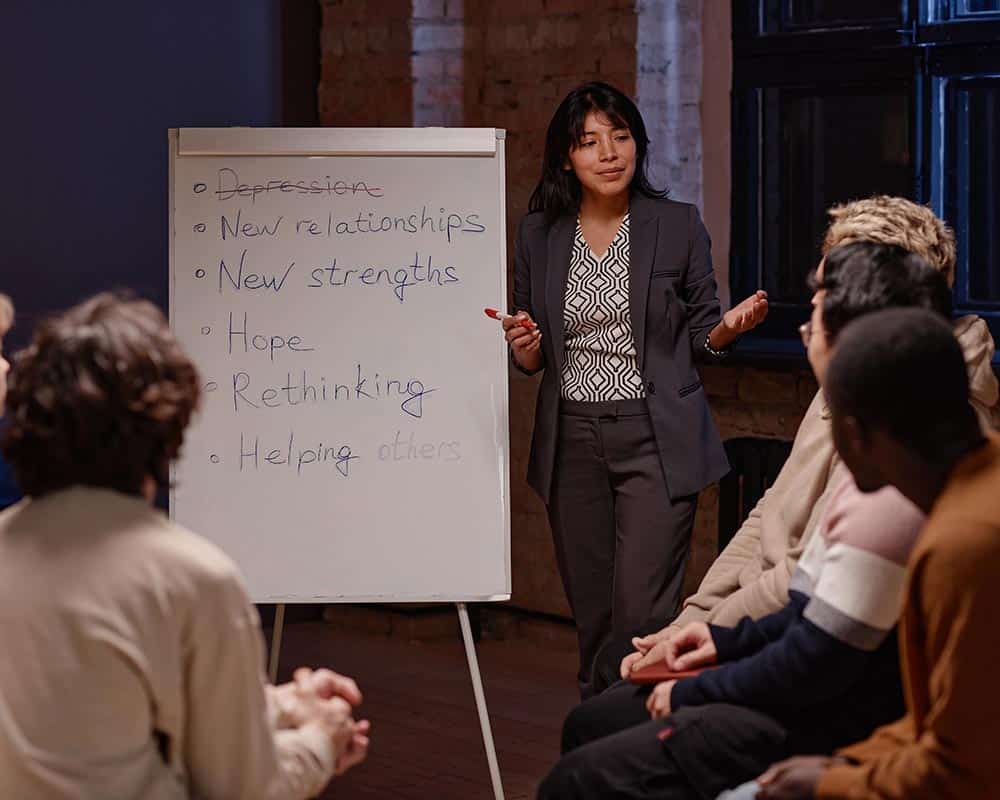
Support Groups and Group Therapy
Group therapy is an effective way for participants to get emotional support from others who have experienced similar challenges in their lives. Additionally, while in groups, individuals learn to expand their ability to build relationships with supportive people in their recovery and to develop a support network.
Some dual diagnosis programs include peer support specialists in the team of individuals who provide support and hope to others. Peer Support Specialists are individuals in recovery from both addiction and mental health conditions who provide hope, practical guidance, and understanding based on lived experience.
Levels Of Care Available For Dual Diagnosis Treatment
A variety of levels of substance use and psychiatric care are available in Massachusetts from dual diagnosis treatment centers.
Residential Treatment For Co-Occurring Disorders
Residential treatment programs provide 24-hour care in a safe and structured environment for individuals with severe co-occurring disorders requiring constant care, those in acute crisis as a result of both their psychiatric symptoms and critical issues with their chemical dependency, people whose living environment is not conducive to a recovery environment, and/or an individual who has failed to be successful in less intensive treatment programs. The purpose of a residential treatment program is for an individual to stabilize both their substance abuse and mental health condition prior to moving to an outpatient treatment program.
Partial Hospitalization Programs (PHP)
Partial hospitalization programs provide the same level of intensity as a hospital inpatient treatment setting, but the person will only be at the treatment center during the day (usually from 5 to 8 hours daily, 5 to 6 days/week). PHP is for individuals who are stepping down from an inpatient treatment program to outpatient treatment, or for an individual with a severe co-occurring disorder who has stable living arrangements, or for individuals in a place where they feel they need more support than standard outpatient treatment provides. In a PHP program, individuals receive the same level of care as inpatient treatment through daily monitoring and therapy, and are allowed to return home in the evenings.
Intensive Outpatient Programs (IOP)
Intensive outpatient programs provide substantial treatment over several weeks while still allowing individuals to fulfill other obligations in their professional, personal, and family lives. Typically, this means participation in at least 3 to 5 days of treatment per week for 9-20 hours/week. This level works well for people with moderate co-occurring conditions and stable support systems, those transitioning from PHP, or individuals beginning treatment who don’t require more intensive care.
Standard Outpatient Treatment
Outpatient treatment continues after completing higher levels of addiction treatment. An example of ongoing outpatient treatment may include monthly appointments with a psychiatrist to monitor an individual’s medication, weekly individual therapy and group therapy appointments, and additional support to help an individual continue their recovery.
Why Integrated Dual Diagnosis Programs Are Effective
Research studies have shown that integrated programs for co-occurring disabilities are more effective and produce greater success than programs that address either the substance abuse or psychiatric disability only.[4]
Studies demonstrate that people receiving integrated co-occurring disorders treatment show better outcomes across multiple measures. They provide:
- Less use and longer abstinence periods from substances
- Decreased psychiatric symptoms, hospitalization, and total number of days in treatment
- Greater compliance with medications and durable improvements in quality of life and function
- Reduced involvement with the criminal justice system
- Increased stability in housing and employment
All of these variables collectively demonstrate that treating persons with both of these disabilities simultaneously produces a synergy of treatment resulting in greater success than treatment of only one of the disabilities.
The integrated approach works because it recognizes that recovery from one condition supports recovery from the other. When a person stabilizes their mental health, it diminishes the urge to self-medicate with substances and provides emotional resources to navigate the challenging issues associated with recovery. When both receive attention simultaneously, people experience more comprehensive healing.
When an individual is treated for one disorder without treating the other, it is rare that an individual achieves long-term sobriety from their substance use disorder. The emotional pain of a psychiatric disability can drive individuals to continue using substances to cope with that pain. Unaddressed substance use prevents psychiatric treatment from working because active addiction interferes with medication effectiveness and therapeutic engagement. Integrated treatment breaks this impasse by tackling both simultaneously.
Start Healing With Dual Diagnosis Treatment in Massachusetts
If you are in Massachusetts and struggling with both drug and mental health problems, you should consider contacting Epiphany Wellness for a comprehensive dual diagnosis approach using a combination of sophisticated, proven, evidence-based therapies, experienced psychiatric intervention, and, most importantly, support from compassionate individuals. We understand that your addiction and mental health are connected, and we treat them that way, with unified care from a team experienced in both addiction medicine and psychiatry.
The clinical team at Epiphany Wellness provides a tailored treatment plan for each individual based upon the unique experience of each client.
Frequently Asked Questions About Dual Diagnosis Treatment in Massachusetts
Begin Your Recovery At Epiphany Wellness
At Epiphany, there is no need for you to select between treating your substance use disorder or your mental health issues because both deserve attention, and both can be treated and healed together. Call Epiphany Wellness’s dual diagnosis treatment centers in Massachusetts today to learn more about the dual diagnosis programs available in Massachusetts, and our admissions staff will gladly answer all your questions, verify insurance coverage, and help you determine which level of treatment is the most appropriate for your individual needs.